Coronavirus Information Relevant to the Forest Products Industry
Last updated 5/29/2020
Key Takeaways
- OSHA has provided a guidance document to assist workplaces in minimizing or preventing the spread of SARS-CoV-2.
- SARS-CoV-2 can persist on surfaces, including packaging materials, from hours to days after contact with an infected individual; it was found to persist approximately 24 hours on cardboard.
- SARS-CoV-2 is inactivated by common biocides such as alcohol (ethanol) and bleach (sodium hypochlorite).
- Standard practices to protect worker health and safety is thought to be effective for SARS-CoV-2 in wastewater treatment operations.
- SARS-CoV-2 is the virus responsible for the respiratory illness known as COVID-19, which is currently in a state of global pandemic.
- Modeling of COVID-19 case statistics provides estimates of peak mortality timeframes that may assist in decision-making for recovery activities as the outbreak subsides. https://covid19.healthdata.org/projections
Resources
Background on Coronavirus | Projections of COVID-19 Impact and Recovery | OSHA Guidance for Preparing the Workplace | SARS-CoV-2 Residency Time on Packaging Materials | SARS-CoV-2 and Wastewater Treatment | References
Introduction
The recent global outbreak of the novel human coronavirus SARS-CoV-2, which has the potential to cause the respiratory illness known as COVID-19, has raised concerns regarding the potential impact of this outbreak on operations and products in the forest products industry. These concerns relate to the potential human to human transmission of this virus in the workplace, the residency time of the virus on various materials and surfaces that an infected worker may come into contact with, and other potential exposure pathways such as wastewater treatment.
This webpage is intended to provide a summary of the best available scientific information regarding transmissibility and exposure pathways of the SARS-CoV-2 virus relevant to the forest products industry. This document does not prescribe any specific actions regarding SARS-CoV-2 and should not in any way be construed as, legal, health or any other form of advice; nor can we attest to the reliability, accuracy or completeness of the information that has been compiled from third-party sources. However, the information presented should assist forest product manufacturers and the general public in their decision-making to minimize or prevent the transmission of SARS-CoV-2.
Background on Coronavirus
The SARS-CoV-2, novel human coronavirus (sometimes referred to as HCoV-19) was first detected in Wuhan, Hubei Province, China in December 2019.1 Human coronaviruses are representative of viruses that produce respiratory illnesses including Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS).2 SARS-CoV-2 produces the respiratory illness known as COVID-19. As of this writing, 166 countries worldwide have reported positive cases of COVID-19 and the World Health Organization (WHO) has classified the disease as a pandemic.3 While the complete clinical features with regard to COVID-19 are not fully known, reported illnesses have ranged from very mild (including some with no reported symptoms) to severe, including illness resulting in death. Most COVID-19 illness is mild, though serious illness and death can occur, particularly in high-risk populations. Those that are considered high risk for serious illness include older people and people of all ages with severe chronic medical conditions including (but not limited to) heart disease, lung disease, and diabetes.4
The characterization of SARS-CoV-2 transmissibility is the subject of considerable study and the resulting information contributes to an evolving understanding of virus behavior. Human to human spread of the disease has been described with an incubation period of between 2 and 10 days from the time of exposure to the display of symptoms.2,5 It is thought that aerosolized droplets from the upper respiratory tract of infected patients, which may contain high viral loads, contribute to the effective human-to-human transmission of this virus. However, current research indicates the virus remains measurable on the surface of inanimate materials on the order of hours to days, which may also serve as a viable transmission pathway.2,6
Current general risk management practices recommended by the Centers for Disease Control (CDC) for the purpose of slowing the spread of SARS-CoV-2 among the general population include1:
- frequent handwashing for at least 20 seconds
- follow state and local restrictions for the attendance of crowded areas
- avoid contact with symptomatic persons and practice general social distancing (e.g. maintaining a distance of 6 feet from other individuals)
- persons exposed to a confirmed case should self-isolate for a minimum of 14 days
For all COVID-19 information from the CDC click here: https://www.cdc.gov/coronavirus/2019-nCoV/index.html
Projections of COVID-19 Impact and Recovery
Updated 7/14/2020
Researchers at the Institute for Health Metrics and Evaluation (IHME), an independent global health research center located at the University of Washington, have submitted a pre-peer reviewed study (found here) that projects the number of severe cases of COVID-19, the health care resource demand, and the time of peak mortality rates across the United States over a 4 month period. While the projections reported in this study have considerable uncertainty, they are potentially useful in assisting with decision-making for recovery planning as the COVID-19 outbreak eventually reaches peaks locally and begins to subside.
The IHME work was conducted using existing case and COVID-19 transmission data combined with statistical modeling techniques to derive projection estimates. Despite the statistical uncertainty associated with these estimates, the modeled projections provide some useful insight as to when the recovery period from the COVID-19 outbreak may occur. IHME has provided a resource at https://covid19.healthdata.org/projections21 that allows users to look up state-specific peak threshold times. These peak threshold times represent the modeled estimated date at which COVID-19 deaths are expected to peak, and then reduce over time, assuming current social distancing practices are maintained. Due to the variety of parameters that potentially impact transmission and mortality related to COVID-19, there is some degree of uncertainty associated with these projections. As an example, the projected number of deaths related to COVID-19 in the United States over a 4 month period is estimated to be 81,114, but this statistic is surrounded by a 95% uncertainty interval ranging from 38,242 deaths to 162,106 deaths over this same period.
Additionally, other modeling approaches exist that suggest alternative predictions in terms of cases, mortality, and timeline of COVID-19. An example is the COVID-19 Hospital Impact Model for Epidemics (CHIME).22 This model is designed to assist hospital administrations with planning for resource demand during the COVID-19 outbreak and the user interface allows for more specific parameterization of model inputs based on local conditions and assumptions (e.g. regional population, doubling time of cases, severity of cases, etc.). In addition to the use of alternative input parameters, the CHIME model also estimates that current intervention efforts (e.g. social distancing) will not be as effective as assumed in the IHME model. To compare between IHME and CHIME predictions, as of April 6, 2020, the IHME model predicts that the peak health care resource use in Washington D.C. occurred on April 3, 2020. However, a scenario run under the CHIME model for the government of the District of Columbia predicts that peak hospitalization will occur on July 1, 2020 (found here). Both models can be run with new data as it emerges, and it is important to check for the latest updates when using these resources in recovery planning. Given that there is no consensus in the estimated recovery timeline for COVID-19, appropriate uncertainty should be applied to the estimates provided by tools such as those described above and contextualized with other relevant information (e.g. such as local quarantine orders, CDC risk assessment guidance, etc.) when planning for operating and recovery scenarios.
Additional tools exist to track the regional incidence of COVID-19 cases. The CDC COVID Data Tracker website (found here) allows users to track United States COVID-19 cases occurring over the last 7 days, cases per 100,000, and deaths per 100,000 at the state level. The Harvard Global Health Institute also provides a tool that reports the 7 day moving average of United States cases per 100,000 at the county level, as well as an approach to assess risk based on the incidence rate of cases (found here). The risk assessment approach is intended to inform policymakers what mitigation practices are needed at various incidence rates and informs the reader what actions may be taken as local COVID-19 cases increase or decrease. Additional regional tracking information may be available from individual state and county departments of health websites.
Whitehouse staff, in collaboration with the CDC, have published guidance for resuming normal operations in the United States, which entails 3 phases to progressively reduce restrictions as monitored data indicates this activity is not likely to cause a resurgence of COVID-19 cases. The criteria (found here) by which restrictions may be lifted in local or regional areas may be helpful for organizations in formulating a plan to resume normal operations.
Guidance for Preparing the Workplace for COVID-19
Updated 7/14/2020
The Occupational Safety and Health Administration (OSHA) provides guidance for workplaces to prepare for the COVID-19 outbreak. The guidance includes the following major areas for the prevention of SARS-CoV-2 transmission7:
- · Planning for potential areas of risk (e.g., work areas of close contact)
- · Preparing basic infection control practices (e.g., handwashing policies, disinfection where needed)
- · Develop policies and procedures to identify and isolate sick individuals
- · Communicate available workplace flexibilities and protections (e.g., remote work policy)
- · Utilize the standard hierarchy of hazard controls (e.g., engineering, administrative, safe work practices, and personal protective equipment)
The OSHA guidance document provides detailed considerations for risk assessment based on job activity and provides guidance for implementing hazard controls based on this assessment. This resource is available on the OSHA website at https://www.osha.gov/Publications/OSHA3990.pdf
OSHA recommends the use of facemasks to help limit the spread of SARS-CoV-2 when employees cannot socially distance at least six feet or need to interact in public spaces where other employees may congregate. The general guidance for facemask use includes:
- It needs to fit snugly but comfortably against the side of the face.
- It should cover the nose, chin, and mouth.
- It is secured with ties or ear loops.
- It should allow breathing without restriction; it should be removed if breathing becomes difficult.
- It can be laundered and machine dried without damage or change in shape or otherwise be disposable after use.
- It must be inspected before wearing and discarded if damaged or change in shape or deformity.
- You must not touch your face after removing the face cover and must wash your hands with soap and warm water and dry them with clean paper towels.
It is important to note that ‘facemask’ refers to a cloth or surgical mask and not a PPE respirator such as an N95 respirator. N95 respirators may be used by choice of the employee without a formal requirement of fit testing or medical clearance. It is recommended that employees who have known contact with SARS-CoV-2 use an N95 respirator. However, if an employer requires an N95 respirator to be worn at the workplace, standard fit testing and medical clearance requirements for respirators apply. Additionally, some N95 respirators are equipped with an expiratory valve to increase the ease of breathing. This type of N95 respirator does not prevent emission of viral particles from an infected person. Therefore, it does not perform the same function of a facemask, which is to limit the spread of viral particles from an infected person, and should not be used.
Several other Environmental Health and Safety (EHS) resources exist that may help employers respond to issues associated with the COVID-19 outbreak.
The CDC provides updated resources for workplaces seeking guidance on disinfection practices after identifying an infected worker (found here), best practices on social distancing and other prevention measures to control the spread of the virus (found here) and special considerations for workers in critical infrastructure (found here). The CDC has consolidated many of these resources in their Resuming Business Toolkit (found here) designed to assist employers in slowing the spread of COVID-19 and lowering the impact in their workplace when reintegrating employees into business settings. This toolkit includes checklists, infographics, and links to resources with QR codes for ease of use with mobile devices.
OSHA guidance relies on CDC recommendations for the disinfection of workplaces. Guidance for non-health care/non-laboratory workplaces focuses on regular cleaning with the disinfection of high contact surfaces by using an EPA registered disinfectant product verified to inactivate coronavirus. High contact surfaces include tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, sinks, etc. For hard surfaces, disinfectants containing 1/3 cup of bleach per gallon of water or of at least 70% ethanol are recommended in lieu of an EPA registered disinfectant if unavailable.
In the instance that an infected worker is identified, it is recommended to close off the area to workers and open doors and windows waiting 24 hours before disinfecting the area if possible. Consider disabling the HVAC system during this time to limit the spread of viral particles throughout the facility if the HVAC system is not designed to limit the spread of aerosolized particles. Then, clean with an EPA registered disinfectant in all areas the infected worker had contact with, using appropriate PPE (e.g. gloves, N95 respirator or mask), and disinfectant products. Once disinfection is completed, healthy workers may return to work. If 7 or more days have passed since an infected worker was present in an area, no additional disinfection is required.
Several other methods of disinfection may be considered by a facility. Disinfectants may be applied as a fumigant provided the label indicates fumigation is a prescribed use. It is not advised to use disinfectants as a fumigant that does not have this use listed on the product label as this means safety and efficacy of the disinfectant applied as a fumigant has not been evaluated and, as such, application in this manner may be neither safe nor effective. Fumigation has the advantage of reaching spaces that may not be reached by conventional wipe disinfection but may also be less targeted to high contact surfaces that require the most direct contact with a disinfectant.
Ultraviolet C (UVC) is used in some scenarios for maintaining the disinfection of spaces. However, UVC has some significant limitations when used as part of a disinfection protocol. First, UVC requires ‘line of sight’ in order to be effective; that is, the UVC radiation must make contact with the surface desired to be disinfected. For instance, UVC light may disinfect the top of a counter surface exposed to the source but would not disinfect the underside of the counter that is not exposed to the UVC. As well, surfaces desired to be disinfected with UVC must be exposed to an appropriate intensity of UVC to inactivate pathogens. Appropriate intensity is a function of the intensity of the UVC source, the distance between the source and the surface, and time. Many consumer-level UVC devices are not regulated and have not been evaluated for efficacy. An important consideration for UVC as part of a disinfection protocol is that people and animals should not be present when UVC is in use due to the potential risk of eye and skin damage, as well as potential cancer risk.
EPA currently recommends against the use of ozone generation for the inactivation of coronavirus as the necessary concentration of ozone required to inactivate pathogens is in excess of public health guidelines for ozone. However, it should be noted that EPA currently has ongoing research programs evaluating the efficacy of UVC, fumigants, ozone, and other disinfectants on a variety of surfaces as presented in a May 27, 2020 webinar found here.
Understanding the fate and transport of particles and droplets produced by infectious individuals can assist in the development of engineering mitigation strategies. A recent presentation by Dr. Linsey Marr from Virginia Tech to the American Society of Civil Engineers reviews the current research regarding particle and droplet physics as it relates to the spread of airborne pathogens, including SARS-CoV-2 (found here). Mitigation strategies based on the known deposition of airborne particles potentially carrying viable virus are discussed.
The American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) has developed guidance on the potential role of HVAC modifications in limiting the spread of aerosol pathogens similar to SARS-CoV-2. These recommendations include Increasing outdoor air ventilation (disable demand-controlled ventilation and open outdoor air dampers to 100% as indoor and outdoor conditions permit) and upgrading central filtration to MERV-13 and adding portable HEPA filtration to reduce the presence of aerosolized pathogenic particles in the air. The full ASHRAE guidance document can be found here.
There are a variety of ways to test workers and surfaces for the presence of SARS-CoV-2. Some workplaces may consider thermal screening as a method for identifying and isolating infected workers. There are two relevant International Organization for Standardization (ISO) standards for thermal employee screening (found here and here). As well, researchers associated with the CDC have reviewed the performance of three infrared thermal detection systems for this purpose (found here).24
As a diagnostic test for people, the CDC recognizes the “Centers for Disease Control and Prevention (CDC) 2019-Novel Coronavirus (2019-nCoV) Real-Time Reverse Transcriptase (RT)-PCR Diagnostic Panel” (described here) to diagnose COVID-19. This test verifies the presence of the genetic material of the SARS-CoV-2 virus but does not need live virus to be present in order for detection to occur (though a positive test in a person typically means they have an active infection). A specimen is taken from an upper respiratory site with a swab, which is then processed by a qualified laboratory.
Swab samples of inanimate surfaces can also be analyzed through RT-PCR to determine if the virus had been present on the surface of interest. However, similar to the test in humans, it is not necessary for the virus to be viable in order to detect the genetic material and non-infectious viral particles may produce a positive result. In order to determine if viral particles obtained from a surface are viable, they must be subjected to a cell culture test to determine if they are capable of infecting a susceptible cell line.
Antibody testing is also available for blood samples taken from people. Antibody testing determines if a person is producing immunological proteins that help fight off the virus. It is important to note that a positive antibody test does not necessarily indicate that a person has COVID-19; e.g. a person who previously had COVID-19 and no longer has the disease (and is no longer capable of transmitting the disease) may continue to produce the antibody for many months. Therefore, the type of test used must be appropriate to answer the desired question. For instance, an antibody test will indicate that a person either has a current or had a previous case of COVID-19, but it cannot determine whether the infection is active or has ended.
Additional Resources for Workplace Preparation
The National Association for Environmental, Health, Safety, and Sustainability (EHS&S) Management, or NAEM, curates resources in the form of publicly available webinars and blog entries that assist businesses with the integration of COVID-19 environmental health and safety practices with business continuity plans. The resources hosted by NAEM may be helpful to businesses seeking to implement the CDC and OSHA guidance presented above in a manner that is consistent with meeting the unique business needs of individual organizations. Their COVID-19 resources can be found here.
EnhesaTM is a global environmental, health and safety consultancy, providing EHS regulatory compliance assurance support to industries worldwide and maintains a website with daily updates on resources, local regulatory updates (including stay-at-home orders that affect local businesses), and other EHS related news regarding COVID-19 that can be viewed here.
The Council of State Governments (CSG) provides informational support to state governments in order to share policies and approaches to policy development. The CSG maintains an updated webpage dedicated to COVID-19 information (found here) and a page specifically dedicated to executive orders in the United States related to COVID-19 policy (found here).
Similar to CSG, MultiState is a state and local government relations company. They are currently maintaining a Google Docs spreadsheet that provides updated State regulatory information related to COVID-19 response, found here.
SARS-CoV-2 Residency Time on Packaging Materials and other Paper Products
second paragraph below added on 5/22/2020
A potential transmission route of SARS-CoV-2 (though, as noted in the OSHA guidance7, not thought to be the primary transmission route) is that of fomite transmission, which is the transmission of the virus from an inanimate object that has come into contact with an infected individual. One factor that determines the risk of transmission through this route is the residency time from which viable virus particles can be recovered from contaminated material.
On May 11, 2020, the CDC updated language on their COVID-19 website (found here) characterizing the potential transmission of SARS-CoV-2 from surfaces as one of the ways the virus is “not spread easily”. Some lay press outlets have speculated as to whether or not this change in language is based on new data or a new perspective at the CDC of SARS-CoV-2 transmissibility. Subsequently, CDC staff have confirmed that this change in language is simply clarification. The current language is consistent with previous statements by the CDC that fomite transmission is not thought to be a primary route of transmission for this virus, remains consistent with OSHA guidance, and that proper handwashing and disinfecting of high contact surfaces remain effective ways of limiting the spread of the virus through contact with surfaces.
On March 23, 2020, the CDC published volume 69 of the Morbidity and Mortality Weekly Report (MMWR) containing the article, “Public Health Responses to COVID-19 Outbreaks on Cruise Ships”. In this article, it is reported, “SARS-CoV-2 RNA was identified on a variety of surfaces in cabins of both symptomatic and asymptomatic infected passengers up to 17 days after cabins were vacated on the Diamond Princess but before disinfection procedures had been conducted (Takuya Yamagishi, National Institute of Infectious Diseases, personal communication, 2020). Although these data cannot be used to determine whether transmission occurred from contaminated surfaces, further study of fomite transmission of SARS-CoV-2 aboard cruise ships is warranted.”
Unfortunately, some lay press outlets have misinterpreted this report to indicate that the SARS-CoV-2 virus is capable of surviving and capable of transmission and infection from surfaces for up to 17 days after contact with an infected individual. However, what is actually indicated in this report is that the genetic material of the virus (e.g. RNA) has been recovered from surfaces within cruise ships up to 17 days after the last potential contact with infected individuals. The presence of genetic material does not indicate that the virus is intact, alive, or infectious, nor does it indicate that the SARS-CoV-2 remains transmissible or infectious on surfaces for a period of 17 days. As noted by the MMWR authors, these data do not indicate that the transmission could, or did, occur from these surfaces.20
Sparse data for SARS-CoV-2 residency times are available, one being a pre-print article in the New England Journal of Medicine by Doremalen et al. (2020) that has not yet undergone peer review.8 However, the authors evaluated the residency time of SARS-CoV-2 on several materials including some relevant to packaging and reported that viable virus could be detected in aerosols up to 3 hours post aerosolization, up to 4 hours on copper, up to 24 hours on cardboard and up to 2-3 days on plastic and stainless steel. The authors concluded that the half-lives of SARS-CoV-2 and the older strain, CoV-1 (which was also tested in this study), were similar except that SARS-CoV-2 did survive longer on cardboard than did CoV-1. However, the authors note that more variability was found in replicates for the result of cardboard, and thus the findings are associated with some uncertainty.
In published correspondence in the Lancet, Chin et al. (2020)23 reports data regarding the impact of environmental conditions on SARS-CoV-2 residency times, specifically evaluating the impact of temperature and relative humidity. The authors reported that no infectious virus could be recovered from printing and tissue papers after a 3-hour incubation, whereas no infectious virus could be detected from treated wood and cloth on day 2 at room temperature (e.g. 22°C) and 65% relative humidity. The authors also note that special laboratory techniques were required to recover the virus from objects and therefore, this recovery of the virus does not necessarily reflect the potential to pick up the virus from casual contact. Consistent with the findings of Doremalen et al. (2020), Chin et al. (2020) reports that residency times were typically longer on smooth, non-porous surfaces. The authors also report that residency times could be substantially extended in low temperatures similar to those found in household refrigerators (4°C). Differences in methods may account for some of the variability observed between these two studies (e.g. application of virus to materials through a nebulizer as in Doremalen et al. (2020) vs. application with a pipette as in Chin et al. (2020)).
Previous studies on CoV-1 (that produces SARS) found similar or slightly extended residence times on paper and wood compared to Doremalen et al. (2020) and Chin et al. (2020). Duan et al. (2003) observed that the CoV-1 virus remained infective after 96 hours of residency on press paper, 120 hours of residency on filter paper, and 96 hours of residency on wood board. However, it is notable that the maximum infectivity observed by Duan et al. (2003) from contaminated paper was less than that of glass or primary exposures such as infected sputum. As well, the infectivity rate at the end of the residency period observed by Duan et al. (2003) was extremely low, in that only a few test cells were observed to be infected with viable virus particles as compared to 26% – 50% of test cells that were infected within the first 48 to 72 hours. Lai et al. (2005) found that residency time was largely dependent on viral concentrations and that the higher concentration tested in their evaluation remained present approximately 24 hours after inoculation and that the lower concentration tested was not found to be present after 5 minutes.9 These findings led Lai et al. (2005) to conclude, “The risk of infection via contact with droplet-contaminated paper is small.”
It is important to remember that these types of fomite transmissions have the potential to occur if the material in question has had substantive exposure to an infected individual shedding virus.
It should be noted that if forest products such as paper products are finished with secondary packaging (e.g., plastic wrap, foil lamination, etc.) that residency times for the relevant packaging materials may be considered for evaluating potential residency times for those products. As well, research conducted with surrogate viruses (gastroenteritis virus and mouse hepatitis virus) suggests that lower temperatures and lower relative humidity have the potential to prolong residency times and higher temperatures and relative humidity have the potential to reduce residency times relative to what is typically experienced in an indoor environment.10
For all surfaces of concern, alcohol (ethanol), bleach (sodium hypochlorite), and glutardialdehyde were observed to be effective biocides and disinfectants for previous strains of coronavirus. Ethanol at concentrations between 62% and 71% reduced coronavirus infectivity within 1 minute of exposure time by several orders of magnitude, to near non-infective levels. Concentrations of 0.1 – 0.5% sodium hypochlorite and 2% glutardialdehyde were also effective with a similar reduction of infectivity. However, it was observed that 0.04% benzalkonium chloride, 0.06% sodium hypochlorite and 0.55% orthophtalaldehyde were less effective.11 The specific susceptibility of SARS-CoV-2 to common biocides is supported by the findings of Chin et al. (2020)23. As well, the EPA maintains a list of biocides that meet their criteria for use against SARS-CoV-2, found here.
WHO has published a protocol12 for public health officials to conduct sampling and analysis of coronavirus on surfaces, which can be found here: https://apps.who.int/iris/bitstream/handle/10665/331058/WHO-2019-nCoV-Environment_protocol-2020.1-eng.pdf
SARS-CoV-2 and Wastewater Treatment
updated on 5/29/2020
SARS-CoV-2 has been detected in the feces of some patients diagnosed with COVID-19. The amount of virus released from the body (shed) in stool and how long the virus is shed is not well characterized, but a case evaluation by Xiao et al. 2020 demonstrated that virus isolated from the stool of an infected patient could viably infect cell culture.25 The risk of transmission of COVID-19 from the feces of an infected person is also unknown. SARS, a similar coronavirus, has been detected in untreated sewage for up to 2 to 14 days. In the 2003 SARS outbreak, there was documented transmission associated with sewage aerosols.13
There are known microbial hazards for workers engaged in managing wastewater treatment operations. The SARS-CoV-2 hazard is expected to be controlled with standard risk mitigation strategies currently employed in wastewater treatment.16 The CDC has provided the following guidance for wastewater treatment workers:12
“Wastewater treatment plant operations should ensure workers follow routine practices to prevent exposure to wastewater. These include using engineering and administrative controls, safe work practices, and PPE normally required for work tasks when handling untreated wastewater. No additional COVID-19–specific protections are recommended for employees involved in wastewater management operations, including those at wastewater treatment facilities.”
The CDC recommends the following “Basic Hygiene Practices for Workers” handling human sewage or waste:14
- Wash hands with soap and water immediately after handling human waste or sewage.
- Avoid touching face, mouth, eyes, nose, or open sores and cuts while handling human waste or sewage.
- After handling human waste or sewage, wash your hands with soap and water before eating or drinking.
- After handling human waste or sewage, wash your hands with soap and water before and after using the toilet.
- Before eating, removed soiled work clothes and eat in designated areas away from human waste and sewage-handling activities.
- Do not smoke or chew tobacco or gum while handling human waste or sewage.
- Keep open sores, cuts, and wounds covered with clean, dry bandages.
- Gently flush eyes with safe water if human waste or sewage contacts eyes.
- Use waterproof gloves to prevent cuts and contact with human waste or sewage.
- Wear rubber boots at the worksite and during transport of human waste or sewage.
- Remove rubber boots and work clothes before leaving the work site.
- Clean contaminated work clothing daily with 0.05% chlorine solution (1 part household bleach to 100 parts water).
Additionally, standard PPE for workers dealing with sewage recommended by the CDC include:
- Goggles: to protect eyes from splashes of human waste or sewage.
- A protective face mask or splash-proof face shield: to protect nose and mouth from splashes of human waste or sewage.
- Liquid-repellent coveralls: to keep human waste or sewage off clothing.
- Waterproof gloves: to prevent exposure to human waste or sewage.
- Rubber boots: to prevent exposure to human waste or sewage.
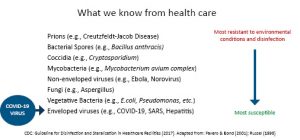
The Water Research Foundation (WRF) has stated SARS-CoV-2 is in the family of viruses most susceptible to environmental conditions and disinfection, as shown in the following diagram:17
The CDC indicates data suggest standard municipal wastewater system disinfection practices may be sufficient to inactivate coronaviruses, including facilities using chlorine where free available chlorine is monitored during treatment to ensure it has not been depleted.15 Previous findings related to SARS indicates that CoV-1 is disinfected when chlorine dosing produces a free chlorine residual between 0.2 and 0.5 mg/L in municipal wastewater.16 The relative susceptibility of viruses similar to SARS-CoV-2 to typical wastewater treatment processes suggests environmental conditions in pulp and paper wastewater treatment systems may reduce virus survival and thus reduce risk to wastewater treatment workers. As a result of the evidence that suggests standard practices are effective in the prevention of COVID-19, the CDC concludes, “No additional COVID-19–specific protections are recommended for employees involved in wastewater management operations, including those at wastewater treatment facilities.18
back to top
References
- Centers for Disease Control. March 7, 2020. Interim US Guidance for Risk Assessment and Public Health Management of Persons with Potential Coronavirus Disease 2019 (COVID-19) Exposures: Geographic Risk and Contacts of Laboratory-confirmed Cases. https://www.cdc.gov/coronavirus/2019-ncov/php/risk-assessment.html
- Kampf, G. Todt, D. Pfaender, S. Steinmann, E. 2020. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection 104:246-51.
- World Health Organization. March 17, 2020. Novel Coronavirus (COVID-19) Situation. https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd
- Centers for Disease Control. March 15, 2020. Situation Summary. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html
- Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020. https://doi.org/10.1016/s0140-6736(20)30154-9.
- Neeltje van Doremalen, Trenton Bushmaker, Dylan Morris, Myndi Holbrook, Amandine Gamble, Brandi Williamson, Azaibi Tamin, Jennifer Harcourt, Natalie Thornburg, Susan Gerber, Jamie Lloyd-Smith, Emmie de Wit, Vincent Munster. 2020. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. New England Journal of Medicine Pre-peer review. https://doi.org/10.1101/2020.03.09.20033217.
- Occupational Health and Safety Administration. 2020. Guidance on Preparing Workplaces for COVID-19. U.S. Department of Labor. OSHA 3990-03 2020.
- Ibid., 2
- Lai MY, Cheng PK, Lim WW. 2005. Survival of severe acute respiratory syndrome coronavirus. Clinical Infectious Diseases 41:e67e71.
- Casanova LM, Jeon S, Rutala WA, Weber DJ, Sobsey MD. 2010. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Applied Environmental Microbiology 76:2712e7.
- Ibid., 2
- World Health Organization. 2020. Surface sampling of coronavirus disease (COVID-19): A practical “how to” protocol for health care and public health professionals. WHO/2019-nCoV/Environment_protocol/2020.1
- Centers for Disease Control and Prevention. 2020. Water Transmission and COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/php/water.html
- Centers for Disease Control. 2015. Guidance for Reducing Health Risks to Workers Handling Human Waste or Sewage. https://www.cdc.gov/healthywater/global/sanitation/workers_handlingwaste.html.
- Ibid., 4
- Xin-Wei Wang, Jin-Song Li, Ting-Kai Guo, Bei Zhen, Qing-Xin Kong, Bin Yi, Zhong Li, Nong Song, Min Jin, Wen-Jun Xiao, Xiu-Mei Zhu, Chang-Qing Gu, Jing Yin, Wei Wei, Wei Yao, Chao Liu, Jian-Feng Li, Guo-Rong Ou, Min-Nian Wang, Tong-Yu Fang, Gui-Jie Wang, Yao-Hui Qiu, Huai-Huan Wu, Fu-Huan Chao, Jun-Wen Li Tsang et al. 2005. Concentration and detection of SARS coronavirus in sewage from Xiao Tang Shan Hospital and the 309th Hospital. Journal of Virological Methods 130:1-2,156-161
- Water Environment Federation, Current Priority: Coronavirus. https://www.wef.org/news-hub/current-priorities/coronavirus/#watersector.
- Water Research Foundation, Coronavirus Disease 2019 (COVID-19) Research Update. March 12, 2020 webcast. https://www.waterrf.org/resource/coronavirus-research-update.
- Ibid., 4
- Centers for Disease Control. 2020. Public Health Responses to COVID-19 Outbreaks on Cruise Ships. Morbidity and Mortality Weekly Report. Early Release, Vol 69. https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6912e3-H.pdf
- IHME COVID-19 health service utilization forecasting team and Christopher JL Murray. 2020. Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. medRxiv 2020.03.27.20043752; doi: https://doi.org/10.1101/2020.03.27.20043752 pre-print; not peer-reviewed
- Predictive Healthcare team at Penn Medicine. 2020. COVID-19 Hospital Impact Model for Epidemics (CHIME). v1.1.2 https://penn-chime.phl.io/
- Chin A W H, Chu J T S, Perera M R A, et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe 2020; published online April 2. https://doi.org/10.1016/S2666-5247(20)30003-3.
- Nguyen, A. V., Cohen, N. J., Lipman, H., Brown, C. M., Molinari, N., Jackson, W. L….Fishbein, D. B. (2010). Comparison of 3 Infrared Thermal Detection Systems and Self-Report for Mass Fever Screening. Emerging Infectious Diseases, 16(11), 1710-1717. https://dx.doi.org/10.3201/eid1611.100703.
- Xiao F, Sun J, Xu Y, Li F, Huang X, Li H, et al. 2020. Infectious SARS-CoV-2 in feces of patient with severe COVID-19. Emerg Infect Dis. 26:8 https://doi.org/10.3201/eid2608.200681
